Many medical providers are plagued by claim denials, billing errors and delayed payments all of which impact their revenue and productivity. Manual processes lead to mistakes, compliance risks and added stress on administrative staff.
In this blog we’ll look at how AI and automation can solve these problems – reduce errors, speed up billing workflows and improve financial performance for medical practices.
The Rise of AI and Automation in Healthcare
AI is no longer just a buzzword. From diagnostics to patient engagement it’s happening across the healthcare industry. In medical billing AI and automation tools are being used to manage administrative tasks, process claims and analyze huge amounts of data faster and more accurately.
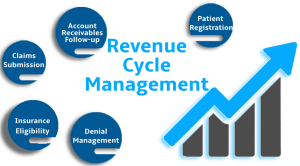
By using machine learning algorithms billing systems can now predict claim outcomes, flag potential errors before submission and ensure accurate coding. Automation tools do the repetitive tasks like patient data entry, eligibility verification and payment posting so billing staff can focus on more strategic work.
Reducing Human Error and Claim Denials
One of the biggest benefits of automation is reducing human error—a common cause of claim denials. AI-driven platforms can spot mismatched codes, missing documentation or incorrect patient info in an instant. They learn from historical data so they get better over time and more accurately.
For medical practices this means fewer rejections and faster payments. According to industry reports automated billing can reduce claim denials by up to 30% so it’s a must have for revenue cycle management.
Enhancing Efficiency and Speed
Speed is key in the billing cycle. The longer it takes to process a claim the longer the wait for payment. Automation reduces turnaround time by handling claim scrubbing, submission and follow ups instantly. It also allows for 24/7 operations so billing can continue outside of regular business hours.
AI can also generate real-time reports and predictive analytics so providers can monitor performance, identify bottlenecks and make informed decisions to improve financial outcomes.
Improved Compliance and Security
HIPAA and payer rules are always on your mind. AI systems stay up to date with those rules and keep your billing compliant. They catch potential issues before they become big problems.
And advanced automation platforms have high level encryption and access controls to protect patient data. So you get high efficiency without compromising security.
Better Patient Experience
Believe it or not automation benefits patients too. Streamlined billing means fewer surprises on their statements, faster resolution of billing disputes and more transparency. AI chatbots can answer billing questions, payment options and insurance coverage without them having to wait on hold for customer service.
By removing billing headaches healthcare providers can increase patient satisfaction and trust—a big deal in today’s competitive healthcare market.
Challenges in Adoption
While the benefits are clear, there are challenges to adopting AI and automation in medical billing. Initial setup costs, staff training and system integration with EHRs and existing workflows can be a barrier for smaller practices. But as the technology gets more affordable and user friendly, adoption will pick up.
Choosing the right partner or billing service provider is key. At ClinicalMDCare, we have AI assisted medical billing solutions for practices of all sizes. Our systems are designed to improve cash flow, reduce denials and be compliant – without overwhelming your staff.
The Future Is Now
AI and automation are no longer optional—they are the new normal in efficient, compliant and profitable billing. As providers are getting more and more administrative and financially burdened, smart billing solutions are timely and necessary. By doing so today, you can protect your revenue and get ahead of the curve tomorrow.