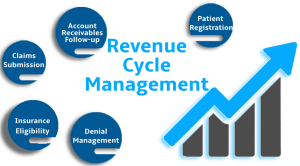
Accurate Medical coding is key in healthcare by converting medical services into standardized alphanumeric codes. These codes describe diagnoses, treatments and procedures performed during patient visits. Insurance companies use these codes to process claims quickly. Without them communication between providers and payers is broken and unclear.
Every treatment, test and diagnosis must be coded correctly to ensure proper documentation and billing. Correct coding also keeps patient histories and clinical records organized. Hospitals use this data for reporting, planning and healthcare improvement. Inaccuracies disrupt these processes and create administrative burdens.
Why Accuracy Matters for Insurance Reimbursements
Accurate medical coding is critical for providers to get full reimbursement from insurance companies. Insurance payers review codes to determine service necessity and pricing. Incorrect or incomplete codes can result in denied or underpaid claims. Providers lose revenue and time correcting these issues.
Insurance companies also flag repeated coding errors as suspicious billing behavior. This can delay future payments. Precision in coding keeps reimbursement flowing and builds trust with payers. It allows providers to keep a healthy cash flow and quality patient care.
Common Coding Mistakes and Their Consequences
Outdated codes, incorrect modifiers or mismatched diagnosis and treatment codes. Small mistakes but big denials. One missing digit or wrong character in a code and reimbursement is delayed or denied.
Frequent mistakes mean ongoing payment disputes and compliance audits. Medical practices lose money and reputation. Patients are affected if services aren’t covered due to coding errors. Accurate coding protects both financial and patient interests.
How Accurate Coding Helps with Compliance and Reduces Legal Risks
Coding must comply with CMS, HIPAA and private insurance rules. Repeated errors look like fraud or abuse. Legal action can follow: fines, payment recoupment or suspension. Providers must ensure their coding is national standards compliant.
Good coding practices promote transparency and reduce the risk of an investigation. Consistent documentation protects against audits and claim disputes. In legal terms it’s a defense that the provider acted in good faith. Compliance is key to long term practice success.
Training and Tools to Improve Coding Accuracy
Ongoing training is key to keep coders up to date on new guidelines and coding changes. Medical coding systems like ICD-10, CPT and HCPCS change regularly. Trained coders know these changes and reduce costly errors. Certified coders provide better documentation support.
Technology also helps with coding accuracy and speed. Tools like Electronic Health Records (EHR) and coding software do real time validation. They alert coders when codes are mismatched or outdated. These systems reduce human error and improve billing workflow.
The Financial Impact of Accurate Coding
Correct coding means timely and full payment from insurance companies. It keeps cash flow steady and predictable for your practice. Denied or delayed claims can kill your practice. Financial stability allows you to reinvest in quality care and staff.
Accurate coding also helps with long term financial planning and reporting. It gives you reliable data to measure practice efficiency. Hospitals and clinics can spot trends, improve services and reduce costs. In short, good coding supports business and clinical outcomes.
Conclusion
Correct medical coding is more than a billing requirement—it’s a requirement for efficient healthcare and survival. Errors delay payment and raise compliance risks. With proper training, modern tools and practice, you can code correctly. And that means revenue, patients and long term success.