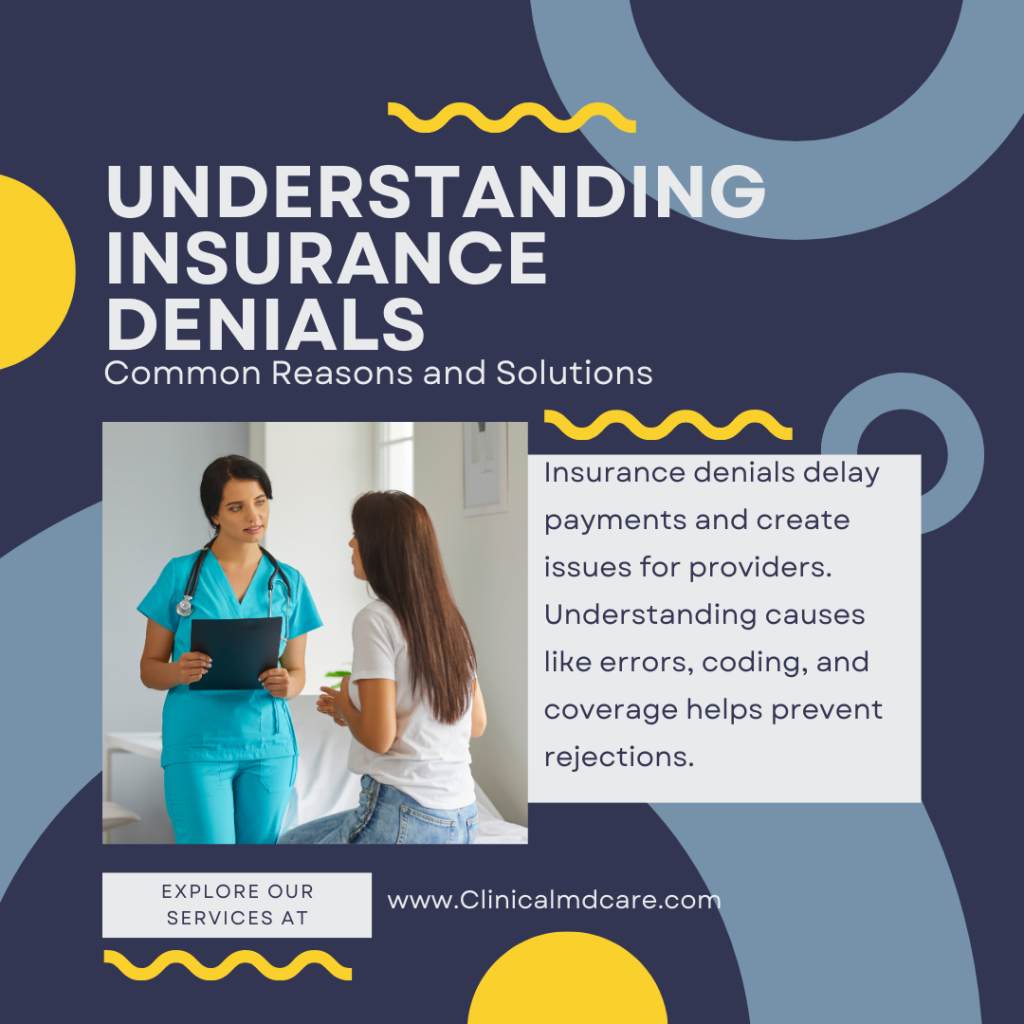
Insurance denials are frustrating for patients and providers. A denied claim means delayed payments and extra administrative work. Knowing why claims get denied helps prevent problems and smooths out the process.
Knowing the common reasons for denials helps you take the right actions. Identifying errors early saves time and money. Let’s look at the most frequent denials and their fixes.
1. Patient Information Errors
Patient information errors are the one of the main reasons for denials. Simple mistakes in names, birth dates or policy numbers cause problems. One incorrect digit in a patient’s insurance ID and the claim gets rejected.
Prevent this by double checking patient info before submission. Verifying with the patient and insurance provider minimizes errors. Using electronic verification tools ensures accuracy and reduces denials.
2. Incomplete Documentation
Missing or incomplete documentation causes rejections. Insurance companies need detailed records to process claims correctly. Insufficient medical records makes it hard to justify treatment.
Avoid this by attaching all necessary documents before submission. Use standardized forms and keep clear concise records. Staff training on documentation practices improves compliance.
3. No Prior Authorization
Some medical procedures require prior authorization before treatment. If prior approval is not obtained the claim will be denied. Insurance providers need to confirm the procedure meets coverage criteria.
Fix this by always checking prior authorization requirements before scheduling treatment. Communicate with insurers to get approval. Implement an internal tracking system to manage authorization requests.
4. Non-Covered Services
Every insurance plan has limitations on covered services. Some treatments are not covered in a patient’s policy. Submitting a claim for an excluded service gets auto rejected.
Review the insurance policy before treatment. Inform patients about uncovered services to avoid confusion. Offer alternative payment options so patients can still get necessary care.
5. Timeliness Issues
Insurance companies have deadlines for claims. Late submissions get auto denied. Each insurer has different deadlines and missing them means lost reimbursement opportunities.
Prevent this by setting up a tracking system for deadlines. Automate reminders to submit claims on time. Audit regularly to catch pending claims before deadlines expire.
6. Coding Errors
Coding mistakes results in insurance denials. Even tiny CPT or ICD code errors can deny a claim. Insurers need exact coding to process claims correctly.
To fix this, use updated coding guidelines and train staff regularly. Hire certified coders to minimize errors. Invest in coding software to increase accuracy and reduce denials.
7. Duplicate Claims
Submitting the same claim multiple times results in denial. Insurers reject duplicate claims to prevent overpayment. Claim tracking confusion often causes accidental resubmission.
To avoid this, implement a central claim tracking system. Train staff to check claim status before resubmission. Use automated claim management tools to reduce duplicates.
8. Out-of-Network Providers
Insurance doesn’t cover services from out-of-network providers. Patients getting treatment from an unauthorized provider risk denial. Many insurance plans have network restrictions.
To prevent this, verify network eligibility before scheduling treatment. Inform patients about coverage limitations ahead of time. Negotiating with insurers for network expansion benefits both providers and patients.
9. Coordination of Benefits Issues
When patients have multiple insurance plans, coordination is key. If benefits aren’t coordinated correctly, claims will be denied. Insurers need clear information on primary and secondary coverage responsibilities.
To fix this, verify the patient’s coverage before submitting a claim. Bill primary insurance first. Educate patients to provide accurate COB information.
10. Medical Necessity Denials
Insurers require proof treatment is medically necessary. If they think a service isn’t necessary, they’ll deny the claim. Lack of sufficient documentation often leads to denial.
To prevent this, provide detailed medical documentation supporting treatment necessity. Include doctor’s notes and test results. Talk to insurers about required documentation to increase approval rates.
Also Read: How AI is Transforming Medical Billing and Claims Processing
Conclusion
Knowing the common denial reasons helps healthcare providers avoid denials. Proactive steps means faster approvals and less financial loss. Efficient claim management benefits both providers and patients.
Strong verification and documentation processes minimizes errors. Staying up-to-date on insurance policies and coding requirements increases approval rates. Taking these steps streamlines the reimbursement process and stability.